Missouri’s pediatric behavioral health crisis

BY TRISH LOLLO, PAUL KEMPINSKI, STEVEN BURGHART and JOSEPH KAHN
The Missouri Times
Since the onset of the COVID-19 pandemic, it has been generally accepted that the virus is not as dangerous to children. Of our nation’s more than 600,000 deaths attributed to COVID-19, nearly 400 have occurred in children ages 0 to 17. For anyone tempted to view this impact dispassionately as “minimal,” we can assure you it is not.
These pediatric COVID statistics obscure the enormity of a shadow pandemic that is pulverizing our country’s kids: the deterioration of mental, emotional, and behavioral health.
Recently, the weekly senior leadership meeting at St. Louis Children’s Hospital was halted when one of its participants received an alert: “I need to inform this group that we have a 16-year-old on campus who our public safety officers believe is at risk of throwing themselves from the top of our parking garage in an apparent suicide attempt.”
Fortunately, the child in this case did not take their own life.
A 14-year-old with no prior history of mental health issues arrived in the emergency room with acute suicidal ideation, having a plan and the means to carry it out. The plan had been discovered after the teen shared a text message with a friend, saying goodbye. Inpatient psychiatric care was needed, but beds at the hospital and throughout the St. Louis region were full. While caregivers searched for available inpatient beds in Columbia, Springfield, Illinois, and beyond, the patient stayed in a small exam room in the emergency department, distraught parents alongside. The patient’s stress and parents’ despair increased by the hour. After 80 hours, an inpatient bed became available in a regional adolescent psychiatric unit. The teen was transferred, but appropriate acute care was initially delayed — time lost toward improving health and well-being.
These are but two examples. Anecdotes like this have become unnervingly commonplace at children’s hospitals in Missouri and across the nation.
Make no mistake: Our current crisis in pediatric mental health was gaining steam well before COVID-19 took hold. Nationwide, the rate of suicide among kids ages 10 to 24 increased by 60 percent from 2007 to 2018. Admissions and emergency room visits for suicide attempts doubled at children’s hospitals from 2008 to 2015. Similarly, visits to children’s hospitals by kids ages 6 to 12 seeking mental health care needs also doubled from 2016 to 2019.
For the last 15 months, kids’ well-documented social isolation and increased family stress have only intensified the troubling pre-pandemic trends in severe mental health conditions such as suicide ideation, self-injury, and substance abuse disorders. The Children’s Hospital Association notes that from April to October 2020, the proportion of mental health emergency department visits increased significantly among kids ages 5 to 11 (+24 percent) and ages 12 to 17 (+31 percent) versus the same period in 2019.
This spring, it’s as if the floodgates broke wide open. Children’s hospital emergency rooms nationwide have become overwhelmed with families in need of immediate help. On average, some of Missouri’s most reputable pediatric health care providers — a group including St. Louis Children’s Hospital, Children’s Mercy Kansas City, SSM Health Cardinal Glennon Children’s Hospital, and Mercy Children’s Hospital St. Louis — saw significant increases in patients presenting to our emergency departments with behavioral health needs vs. the same period in 2019.
The implications for the timely, appropriate, and safe care of kids with mental health needs are multifaceted.
1. At present, the demand for pediatric mental health services far exceeds the available supply. This applies to both human and physical resources. On the former, there simply aren’t enough specially trained health care providers to care for this population of kids. The CHA estimates our nation has a demonstrated need for 47 child psychiatrists per 100,000 kids and teens. Currently, there are 10 child psychiatrists per 100,000. On the latter, hospitals lack the number of inpatient beds and opportunities for placement externally to provide appropriate and safe care to patients whose needs are the most acute.
2. Children’s hospitals are not equipped to care for patients with mental health needs at scale. Because there is a dearth of specialty providers for these kids, children’s hospitals are bearing the brunt of the volumes because, in some cases, our emergency departments are a child or family’s only refuge. Holding kids with mental health needs in our emergency rooms — often for 24 hours or more — while waiting for an inpatient bed to become available is not therapeutic. Stimulation from a busy and sometimes chaotic environment can increase their levels of anxiety and agitation. It frequently results in a worsening of symptoms, a higher risk of harm for both patients and staff, and a greater likelihood of elopement — defined as patients leaving the hospital when doing so may present an imminent threat to their safety.
3. “Safe care” is a two-sided coin. Children’s hospitals — and more specifically, the people who work at them — exist to take care of our communities’ most vulnerable kids at their times of greatest need. But even those who thought they knew what they signed up for — the triumph, the heartbreak, the risk — couldn’t have imagined this. Our most highly acute patients can be a threat to themselves, but also to our staff. Patients who are in crisis do not always know how to express themselves. At times they lash out, and several have inflicted extensive harm on many of our frontline team members. With the growing shortage of health care workers across the country, especially in the state of Missouri, we need to do everything we can to protect our staff from harm, while also ensuring that our patients are receiving the highest-level care.
As a group, Missouri’s children’s hospitals continue to highlight the need for immediate federal, state, and local support to help providers meet the demand of our kids, our families, and our communities. We believe that long-term solutions are needed to address decades of chronic underinvestment in pediatric mental health services and infrastructure. We have begun to convene various stakeholders in behavioral health to explore potential solutions and look forward to bringing providers, patient advocates, and the state together to craft a best-in-class approach to addressing the behavioral health needs of our communities.
Our kids, families, and communities deserve better.
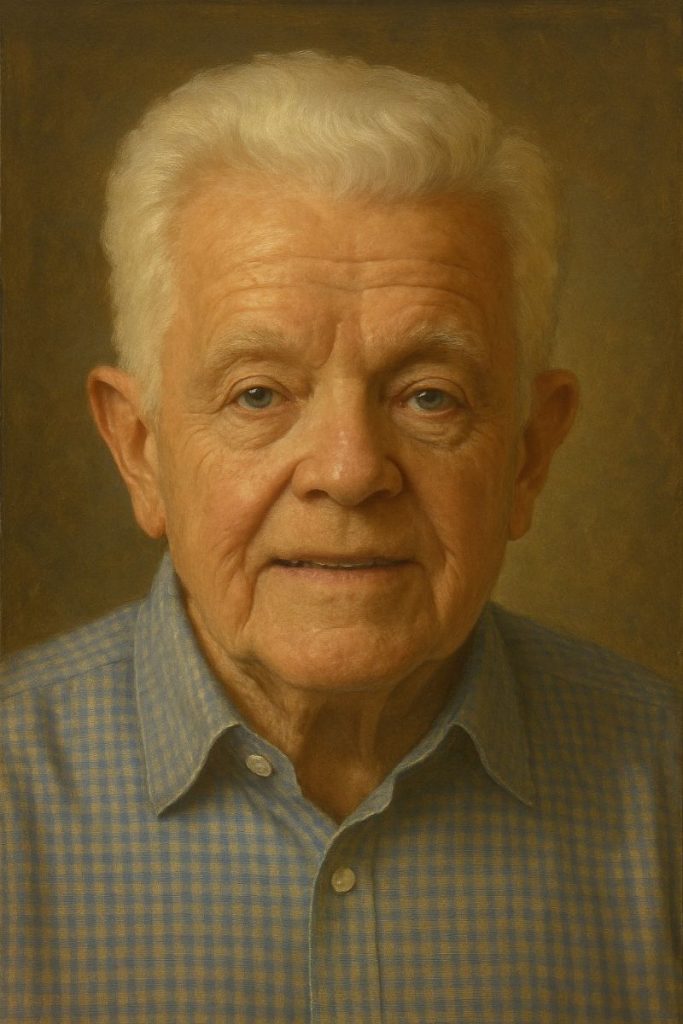
Trish Lollo is the president of the St. Louis Children’s Hospital. Paul Kempinski is the president & CEO of Children’s Mercy Kansas City. Steven Burghart is the president of SSM Health Cardinal Glennon Children’s Hospital. Joseph Kahn, MD, is the president of Mercy Children’s Hospital St. Louis.
Miss Clipping Out Stories to Save for Later?
Click the Purchase Story button below to order a print of this story. We will print it for you on matte photo paper to keep forever.